Today’s news, dominated every day by the COVID-19 pandemic, is often centered on the impact of this virus on seniors living in skilled nursing and seniors housing communities. While an ocean of print is lapping at every front page in the world, regulators and policy makers have rushed to enact new measures to protect frail elders, who are most susceptible to this disease. The resulting disruption that is occurring, and which we see reflected in every news outlet, will have a lasting impact on the sector.
Reflecting back on the news that NIC continues to curate on our www.seniorcare.nic.org resources page, it is possible to see how the headlines trace this period of disruption – and how this crisis will shape the delivery of healthcare in seniors housing for years to come.
Before COVID-19, the sector was already moving towards healthcare partnerships and innovation in numerous ways. A January 15 Senior Housing News story, “Welltower CEO Touts Expanding Health System Initiatives, Teases ‘Welltower Living’ Brand,” highlighted how important healthcare was becoming, before the crisis hit. Writer Tim Mullaney opened the piece with:
“Welltower is moving forward on all cylinders with its strategy of closely aligning senior housing with health systems. In addition to a recently announced relationship with Jefferson Health, the real estate investment trust (REIT) is in the process of working closely with Geisinger Health in Pennsylvania, CEO Thomas DeRosa said Wednesday at the J.P. Morgan Healthcare conference in San Francisco.”
Referring to DeRosa, Welltower CFO Tim McHugh was quoted as saying, “Tom often says that we’re a health care company that expresses our view of where health care is going through our ownership of real estate.”
As hundreds of visitors to our curated headlines section know, many stories were already casting light on a movement to break down old silos and forge new partnerships, secure new technology, and collaborate with healthcare partners.
Reporter Chuck Sudo’s story, “Brookdale Eyes Health System Opportunities as Assisted Living Turns a Corner,” published by Senior Housing News February 19, focused on the management decisions driving assisted living into the healthcare continuum.
Discussing the strategic hiring of Cindy Kent as executive vice president and president of its senior housing arm, Brookdale CEO Cindy Baier said, “With the changes happening in health care moving from fee-based services to pay for performance, there are better opportunities to partner with health systems to make assisted living a part of the care continuum. Having someone [like Kent] who worked in other aspects of the spectrum is important,” Baier told SHN.
Covering the 2020 NIC Spring Conference, on March 10, Globe Street writer Natalie Dolce submitted the article, “NIC 2020 Talks Future of Healthcare Disruption, Scale Will Matter.” The piece focused on NIC Founder and Strategic Advisor Robert Kramer’s remarks. At the time there was dawning awareness of COVID-19 in the U.S., but no one who knows Kramer was surprised to hear his argument that a period of disruption, converging housing and healthcare, and forging innovation and new models, was upon us.
As Dolce reports, “He explained that healthcare players traditionally involved in creating networks to provide acute care are expanding to emphasize wellness, care coordination, and management of chronic conditions to prevent acute care episodes. ‘The reality is that things are changing. We have an enormous opportunity and we are part of the discussion.’” Kramer may not have known how quickly things were, in fact, about to change.
Only 12 days later, stories on CMS’ decision to expand coverage for telehealth, as a means to combat COVID-19, were appearing. Tim Regan’s March 17 Senior Housing News story, “New CMS Telehealth Expansion Could Be ‘Very Good’ for Senior Living During Covid-19,” pointed to the need for this technology in seniors housing:
“’Any expansion of telehealth services is a very good thing,’ Kari Olson, chief innovation and technology officer for Glendale, California-based senior living provider Front Porch, told Senior Housing News. “Especially during this time when we need folks to stay home, and in particular, to safeguard people over 65 as well as other high-risk individuals.”
Regan’s story closes with the observation that, “Many within the industry have touted the promise of telehealth in senior living settings, and this expansion could serve to demonstrate its value in the real world. Medicare Advantage (MA) policy changes enacted last year already make it easier for senior living residents to receive care such [sic]in the independent living or assisted living community where they live rather than in a health care facility.”
By the end of the month, telehealth had become a far more accessible and long-term fixture across the seniors housing and care sector. Alex Spanko’s March 31 Skilled Nursing News’ piece, “Skilled Nursing Telehealth Adoption Not Without Challenges — But COVID-19 Changes Likely Here to Stay” reflects a new reality.
Spanko interviewed Dr. Grace Terrell, CEO of the skilled nursing-focused physician group Eventus WholeHealth, about their roll out of telehealth programs in 500 facilities. “I don’t think you’re going to be able to put the toothpaste back in the tube,” Terrell said. “We’re not going to go back; things will change.”
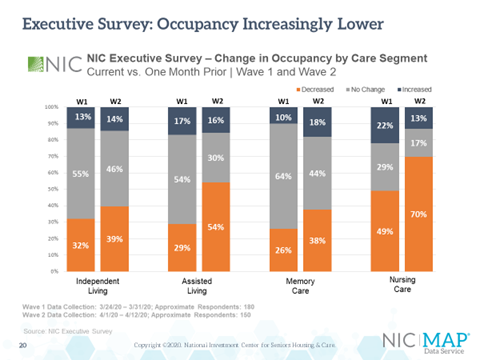
Throughout the month of April, there was a flood of headlines concerning COVID-19. Given the pandemic’s impact on the seniors housing and care sector – and the millions of frail elders in its care – NIC launched its NIC COVID-19 Resource Center, along with numerous initiatives designed to collect and analyze relevant data, disseminate information, host public discussion, and facilitate meetings amongst peers and experts.
We recommend visiting the NIC COVID-19 Resource Center, where you can subscribe to the new “NIC Weekly Recap: COVID-19 Newsletter” for all the latest information and developments relevant to the pandemic. You will also find recordings and summaries for the highly popular “NIC Leadership Huddle” webinar series, and can access results and analysis for the “Executive Survey Insights,” which provides unique insights into the impact of the pandemic across the sector.
Of course, we will continue to curate articles relevant to the developing trends in healthcare innovation, collaboration, and partnerships which continues to shape the future of the sector. News is developing very quickly, as is the impact of the COVID-19 pandemic, and NIC remains committed to keeping you informed as it develops. As we are all seeing in real-time, today’s headlines are outlining the shape of a new normal in the months and years ahead.